A consensus panel convened by the National Institutes of Health (NIH) today concluded there is clear evidence that needle acupuncture treatment is effective for postoperative and chemotherapy nausea and vomiting, nausea of pregnancy, and postoperative dental pain.
The 12-member panel also concluded in their consensus statement that there are a number of other pain-related conditions for which acupuncture may be effective as an adjunct therapy, an acceptable alternative, or as part of a comprehensive treatment program. but for which there is less convincing scientific data. These conditions include but are not limited to addiction, stroke rehabilitation, headache, menstrual cramps, tennis elbow, fibromyalgia (general muscle pain), low back pain, carpal tunnel syndrome, and asthma.
"We need more high quality research to validate what appears to be useful for the millions of Americans that have used acupuncture in this country. The challenge in studying acupuncture is to integrate the theory of Chinese medicine into the conventional Western biomedical research model and into the conventional health care arena," said panel chairman David J. Ramsay, D.M., D. Phil., president of the University of Maryland, Baltimore.
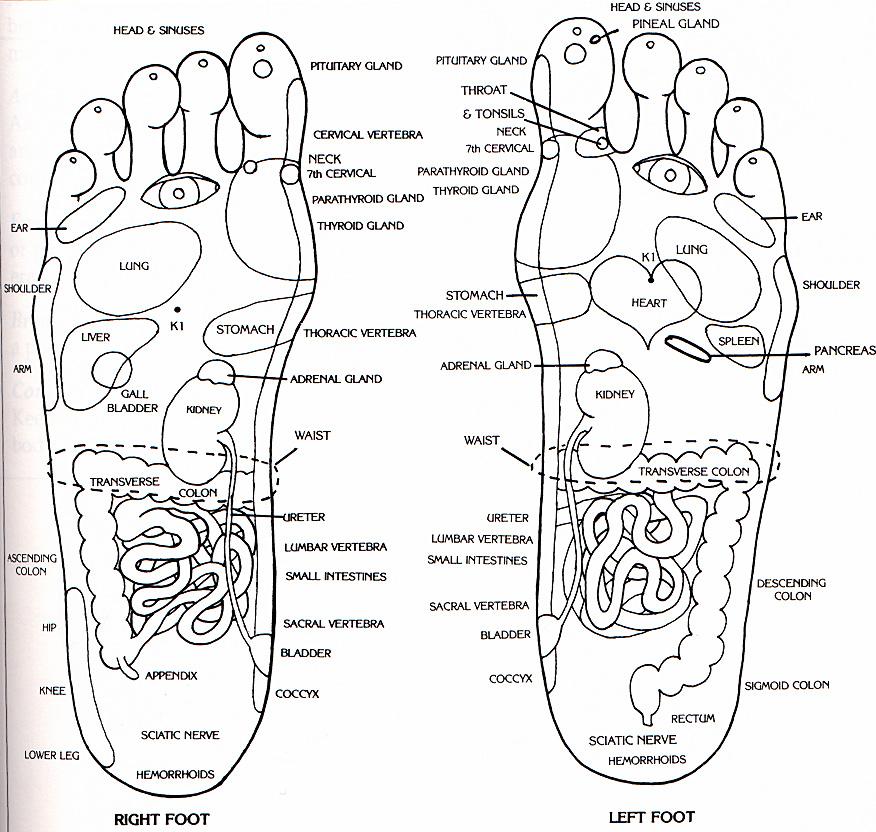
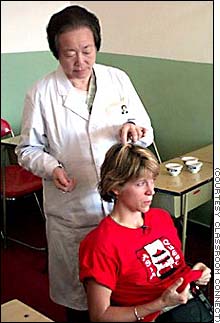
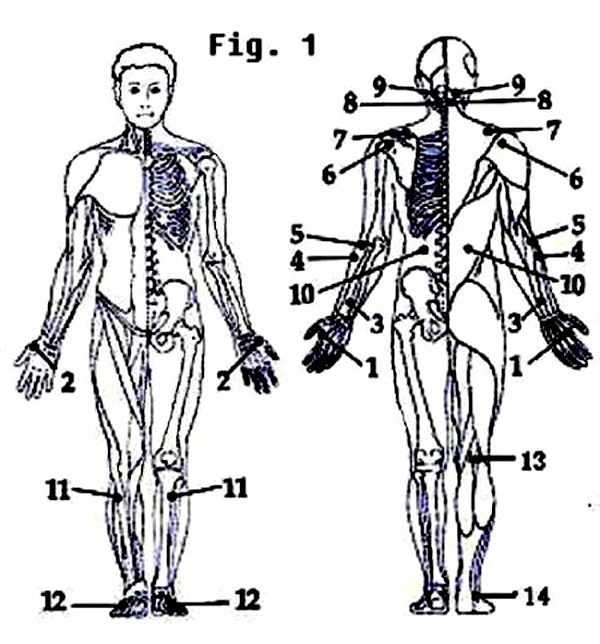
Acupuncture is a family of procedures, the most well known of which involves penetration of specific anatomic locations on the skin, called acupuncture points, by thin, solid, generally metallic needles.
Acupuncture is one of the oldest and most commonly used forms of traditional medicine in the world--dating back for at least 2,500 years. The general theory of acupuncture is based on the premise that there are patterns of energy flow called Qi (pronounced "chee") throughout the body that are essential for optimal health.
Public awareness and use of acupuncture increased in the United States following President Nixon's visit to China in 1972 and New York Times reporter James Reston's account of how physicians in Beijing eased his post-surgery abdominal pain with needles. According to the World Health Organization, there are approximately 10,000 acupuncture specialists in the U.S., and an estimated 3,000 practicing acupuncturists are physicians. In 1993 the Food and Drug Administration reported that Americans were spending $500 million per year and making approximately 9 to 12 million patient visits for acupuncture treatments.
The introduction and acceptance of any new treatment can be a difficult process. When that new treatment is based on theories unfamiliar to Western medicine, the difficulties are accentuated. To enhance the acceptance of acupuncture in the U.S., the panel emphasized the need for improved understanding of perspectives between acupuncture practitioners and today's conventional health care community. The panel commended the ongoing increase in improved training and called for more uniform licensing, certification, and accreditation of acupuncturists among States, which will help the public identify qualified acupuncture practitioners and to have more assurance in quality of service. Thirty-four states license or otherwise regulate the practice of acupuncture by nonphysicians, and have established training standards for certification to practice acupuncture.
Adverse side effects of acupuncture are extremely low and often lower than conventional treatments. However, the panel noted that adverse side effects have occurred on rare occasions. They recommended that patients be fully informed of their treatment options, expected prognosis, relative risk, and safety practices to minimize the risks prior to undergoing acupuncture treatment. Because many individuals seek health care treatment from both acupuncturists and physicians, the consensus panel advocated a strengthening of communications between these health care provider groups to maximize the possibility that important medical problems are not overlooked. The panel additionally encouraged broader public access to acupuncture treatment by urging insurance companies, Federal and state health insurance programs including Medicare and Medicaid, and other third party payers to expand their coverage to include appropriate acupuncture treatments. Doing so, the panel stated, would help remove the financial barriers to access to these services.

The panel issued their consensus statement following an extensive review of the existing medical literature and a series of presentations by acupuncture research experts at a 3-day NIH Consensus Development Conference on Acupuncture. The full NIH Consensus Statement on Acupuncture is available by calling 1-888-NIH-CONSENSUS (1-888-644-2667).
The National Institutes of Health Consensus Development Program was established in 1977 and is the premier health technology assessment and transfer program in American medicine. Under this program, the Office of Medical Applications of Research at NIH organizes major conferences that produce consensus statements and technology assessment statements on controversial issues in medicine important to health care providers, patients, and the general public.
This conference was sponsored by the NIH Office of Medical Applications of Research and the NIH Office of Alternative Medicine. The conference was cosponsored by the National Cancer Institute, the National Heart, Lung, and Blood Institute, the National Institute of Allergy and Infectious Diseases, the National Institute of Arthritis and Musculoskeletal and Skin Diseases, the National Institute of Dental Research, the National Institute on Drug Abuse, and the NIH Office of Research on Women's Health.
To get the The full NIH Consensus Statement on Acupuncture, please click the following pdf file:
NIH Panel Issues Consensus Statement on Acupuncture
NIH Panel Issues Consensus Statement on Acupuncture



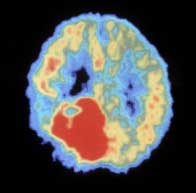
 Those seeking it out include people like research scientist Amy Howell of Rutgers University. After suffering from West Nile virus two years ago, Howell began having serious dissy spells. Western specialists told her the cause was "probably multiple sclerosis or a brain tumor," but they were unable to fix the problem. Finally, in desperation, she turned to an acupuncturist in Cherry Hill, N.J. He diagnosed "stagnant liver qi" and administered acupuncture and herbal remedies. Seven months later Howell's dizzy spells are gone. So are her allergies and a chronic shoulder problem. "I'm a scientist," says Howell. "This doesn't make sense, but there's something there".
Those seeking it out include people like research scientist Amy Howell of Rutgers University. After suffering from West Nile virus two years ago, Howell began having serious dissy spells. Western specialists told her the cause was "probably multiple sclerosis or a brain tumor," but they were unable to fix the problem. Finally, in desperation, she turned to an acupuncturist in Cherry Hill, N.J. He diagnosed "stagnant liver qi" and administered acupuncture and herbal remedies. Seven months later Howell's dizzy spells are gone. So are her allergies and a chronic shoulder problem. "I'm a scientist," says Howell. "This doesn't make sense, but there's something there".


 I decided to give Tai Chi a try. I simply joined in on one of the many groups of people moving and exercising. We stepped rhythmically in turning patterns, swaying our arms as if we were moving an imaginary beach ball. It was easy to get the basics, and though I stood out like a sore thumb in my red pile jacket, the Chinese elders welcomed me. When I was done, I felt like I not only moved my Chi, I loosened my limbs, got my heart pumping, and made a few new friends.
I decided to give Tai Chi a try. I simply joined in on one of the many groups of people moving and exercising. We stepped rhythmically in turning patterns, swaying our arms as if we were moving an imaginary beach ball. It was easy to get the basics, and though I stood out like a sore thumb in my red pile jacket, the Chinese elders welcomed me. When I was done, I felt like I not only moved my Chi, I loosened my limbs, got my heart pumping, and made a few new friends.



 A UBC researcher has shown that acupuncture treatment can be used to reduce substance use among addicts in Vancouver's Downtown Eastside (DTES).
A UBC researcher has shown that acupuncture treatment can be used to reduce substance use among addicts in Vancouver's Downtown Eastside (DTES).




 Scientists have known for years that the most troublesome health problems plaguing Westerners -- heart disease, diabetes, obesity and cancer of the breast, colon and prostate -- are far less common in China. For every 5 American women who die of heart trouble, only one Chinese woman suffers the same fate. The disease kill 17 times more middle-aged men in United States than in China. And China has the lowest rate of breast cancer in the world.
Scientists have known for years that the most troublesome health problems plaguing Westerners -- heart disease, diabetes, obesity and cancer of the breast, colon and prostate -- are far less common in China. For every 5 American women who die of heart trouble, only one Chinese woman suffers the same fate. The disease kill 17 times more middle-aged men in United States than in China. And China has the lowest rate of breast cancer in the world.